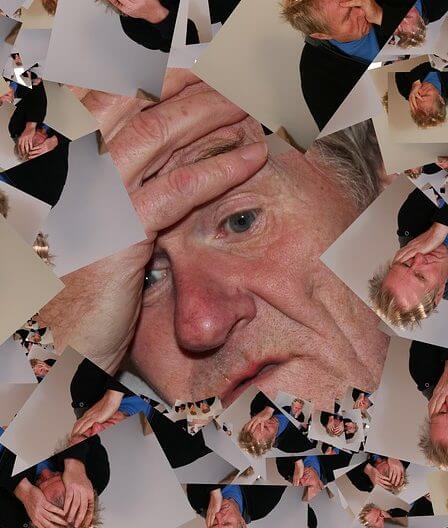
Dementia vs. Delirium: Get to Know the Key Differences!
Dementia and delirium are two terms that often get mixed up, but they’re different things. In this blog post, we’ll break down what dementia and delirium are, what causes them, and how they show up. By the end, you’ll have a clearer picture of the distinctions and similarities between the two.
Dementia: The Basics

Dementia is not a single disease; instead, it’s a group of conditions that affect memory, thinking, and social abilities. It’s like the brain’s ability to do its job is slowly fading away. Alzheimer’s disease is the most common type of dementia, but there are others, like vascular dementia and frontotemporal dementia.
Causes of Dementia
Dementia usually happens when brain cells are damaged. This damage can be due to various factors, like Alzheimer ‘s-related brain changes, vascular issues affecting blood flow to the brain, or certain proteins causing trouble. Age is a significant factor, and most people with dementia are older, but it’s not just a normal part of aging.
Symptoms of Dementia
Spotting dementia involves noticing changes in memory, communication, and daily activities. Someone with dementia might forget things often, struggle to find the right words or find it hard to complete familiar tasks. Personality changes can occur, and they may withdraw from social activities.
Delirium: The Basics
Delirium is more like a sudden, intense confusion. It comes on fast and can fluctuate throughout the day. Unlike dementia, delirium is usually reversible once the underlying issue is treated. It’s a bit like a mental ‘short circuit.’
Causes of Delirium
Delirium is often a sign that something else is wrong in the body. It can result from infections, medication side effects, or changes in the body’s balance of substances like sodium. It’s common in hospitals, especially among older people, and can be triggered by surgery or illness.
Symptoms of Delirium
Delirium symptoms can be quite noticeable. People experiencing delirium may seem confused, have trouble paying attention, or see things that aren’t there. Their thinking might jump around, and they might act agitated or withdrawn. It’s like their mind is in a state of chaos.
Dementia vs. Delirium: Differences
Now, let’s get to the nitty-gritty of how dementia and delirium differ.
Onset and Duration
Dementia creeps in slowly and progressively, often over months or years. Delirium, on the other hand, hits fast, usually within hours or days. Dementia is a long-term deal, while delirium is more of a temporary state.
Reversibility
Dementia is usually irreversible. Once those brain cells are gone, they don’t come back. Delirium, though, can often be reversed. Treat the underlying cause, and the confusion tends to clear up.
Attention and Alertness
People with dementia typically have a steady level of attention and alertness. They might have good days and bad days, but the overall state remains. Delirium, however, can cause sudden shifts in attention and alertness, making someone seem ‘out of it’ one moment and clearer the next.
Dementia vs. Delirium: Similarities
Despite their differences, dementia and delirium share some common traits.
Cognitive Impairment
Both conditions mess with a person’s thinking. Dementia does it slowly over time, while delirium does it rapidly. But in both cases, you’ll notice changes in memory, language, and problem-solving skills.
Behavioral Changes
Dementia and delirium can both bring about shifts in behavior. Someone with dementia might become withdrawn or show signs of aggression. Delirium can lead to restlessness or irritability, making the person act out of character.
Challenges in Daily Activities
Both conditions can make daily tasks tough. For someone with dementia, it’s a gradual struggle. For someone experiencing delirium, it’s more sudden and severe. Simple things like getting dressed or preparing a meal become challenging.
What Does the Research Say?
In this study conducted by researchers Bhanu Gogia and Xiang Fang, the focus was on differentiating between two significant cognitive disorders: dementia and delirium. It was emphasized that not only is it important to distinguish delirium from dementia, but also crucial to recognize the occurrence of superadded delirium in individuals already diagnosed with dementia. This distinction is vital because the presence of delirium in dementia patients can lead to various adverse outcomes.
The study highlighted that when delirium is superimposed on pre-existing dementia, it results in a prolonged length of hospital stay for the affected individuals. Moreover, there is an acceleration in cognitive and functional decline observed in these patients.
This not only has implications for the individual’s well-being but also leads to increased healthcare costs. Ultimately, the study found a correlation between the occurrence of superadded delirium in dementia patients and a higher likelihood of mortality.
For patients diagnosed with delirium, the prognosis is generally guarded. The study underscored that delirium is preventable in approximately 30% of cases. This prevention is particularly significant, considering the serious consequences associated with delirium, such as increased mortality rates.
The research pointed out that there is up to 2 to 4 times higher mortality in patients developing delirium in the intensive care unit (ICU) setting. Additionally, there is a notable up to 1.5-fold increased risk of death within a year following hospitalization for individuals admitted to general medical services, geriatric services, and nursing home residents. This elevated risk is observed especially in those with comorbidities like stroke and dementia.
In simpler terms, the study highlights the importance of distinguishing between dementia and delirium, as well as recognizing the additional impact of delirium in individuals already diagnosed with dementia.
The findings emphasize the serious consequences of superadded delirium, including prolonged hospital stays, accelerated cognitive decline, increased healthcare costs, and a higher risk of mortality. Furthermore, the study suggests that proactive measures to prevent delirium can significantly improve outcomes for affected individuals.
Conclusion
In a nutshell, dementia and delirium may seem similar at first glance, with confusion and behavioral changes, but they have different causes, progressions, and outcomes. Dementia is a long-term decline, while delirium is a temporary state often linked to an underlying issue.
Understanding these differences is crucial because it guides how we approach care and treatment. Dementia requires ongoing support and management, whereas delirium demands a quick investigation into the root cause and addressing it promptly. Both conditions impact not just the individual but also those around them, making awareness and empathy key in providing effective care.
So, the next time you hear these terms, remember: dementia is a slow fade, and delirium is a sudden storm. Each needs its unique approach to understanding and support.
